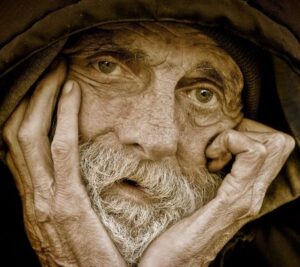
The Case of Jesse, Unrepresented and Homeless
Print this case study here: The Case of Jesse, Unrepresented and Homeless
The Case of Jesse – Unrepresented and Homeless
A 60-year-old homeless man, “Jesse,” is found confused and in distress by a passerby who calls 911. Paramedics bring the man to the hospital. Jesse’s feet and legs are swollen and covered in ulcers and dead tissue—diagnosed as osteomyelitis or infection of his legs.
Paramedics bring the man to the hospital. Jesse’s feet and legs are swollen and covered in ulcers and dead tissue—diagnosed as osteomyelitis, or infection of his legs. His past medical history is established to include chronic obstructive pulmonary disease (COPD), chronic foot infections, alcoholism, and tobacco use. In addition to this, clinicians find a mass in Jesse’s lung that could either be TB or cancer. Physicians recommend a biopsy. The infections in this patient’s legs are so severe that a double amputation is recommended, also.
Jesse says “No!” to amputation, but reluctantly agrees to a biopsy of the lung mass. Then a psychiatric consultation leads to an opinion that the patient actually lacks capacity for healthcare decisions. Jesse had been able to identify his location in a hospital but not why, or what could happen as a result of not going along with medical recommendations for treatment. He had stated to the psychiatrist that he just wants to leave the hospital and die. But does he? Maybe. In a previous hospital admission, the chart indicates that Jesse had refused surgery as treatment for recurring infection in his legs, and physicians believed he had done so with decisional capacity.
Jesse’s support system initially seems to consist only of a couple recent acquaintances at the homeless shelter (who don’t have telephones and cannot be reached) and a dog that Jesse says is his very best friend. A hospital social worker searches for any next of kin, someone who knows Jesse and might be willing and able to make decisions as a surrogate. Social work eventually finds an out-of-town brother and an estranged sister. Neither have seen their brother in many years, and anyway are unwilling to make decisions on his behalf. The attending physician wonders aloud what should be done for Jesse now, and who can decide?
An ethics consultation is requested and received. An ethics note placed in the chart later that day offers several recommendations following a summation of the situation. This is a case seen by ethics as one involving an unrepresented patient without advance directives and a care team with beneficent intent and insufficient information to know exactly what actions would constitute respect for the patient’s autonomy, such as it is, or his best interests otherwise.
Ethics recommendations include:
• convene a multidisciplinary patient care meeting to foster communication amongst multiple care teams
• periodic reevaluation of the patient’s capacity given that it could be an acute rather than chronic state
• continue to update Jesse on his situation so as to respect whatever autonomy he retains or regains www.PracticalBioethics.org
• consider whether there might be other sources of infection, such as TB, that are contributing to his recent loss of decisional capacity and impeding recovery
• reiterate with nursing staff the need for infection control for the safety of care providers and other patients Jesse is stabilized and remains hospitalized for another week. The lung biopsy shows evidence of a lung cancer that is treatable but not curable. Reevaluation of capacity for decision-making indicates that the patient has regained capacity sufficient for decisions for or against treatment of his cancer and infections. Jesse chooses to leave the hospital without further treatment.
Upon discharge, he refuses also to be taken either to a homeless shelter or the nursing home placement that Social Work had found as the recommended discharge option. Jesse is discharged to the street, as he wishes.
Questions for Discussion:
• Is Jesse making the right decision to leave the hospital without treatment? How would we know what the right decision is in this case?
• How should the patient’s medical history, including his history of treatment refusal, impact decision-making during the period when he lacked decisional capacity?
• What justification might have been found to do the recommended amputations over Jesse’s incapacitated objections?
• Might that course of action have been justified if the leg infections were determined to be the primary cause of his acute decisional incapacity?
• What other recommendations might have come from ethics consultation?
• Treatment refusals—whether reasonable or unreasonable (and how would Jesse’s be categorized?) can be emotionally difficult for members of the care team. What should be done to support this care team in light of Jesse’s decisions?
Prepared by:
Clint Cole, B.S., D.O. student
Leslie McNolty, D.P.S.-Bioethics
Tarris Rosell, Ph.D., D.Min.


