Category / Blog / Resources / What's New
-
Ethics Dispatch August 2025
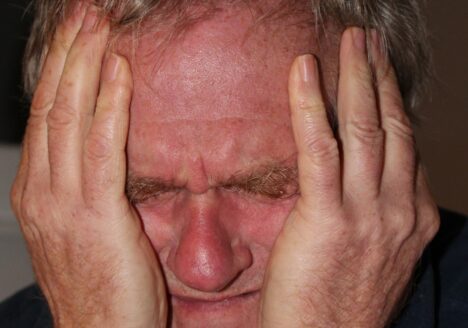
Nurses and frontline staff bear the brunt of a growing wave of hostility, facing risks that extend far beyond the usual emotional toll of caregiving. In this Ethics Dispatch, the Center for Practical Bioethics analyzes competing values that govern providers’ response to violence, as well as institutional responsibilities and Ryan shares a personal story about his response to an aggressive family member.
-
Case Study – Doctor-Patient Relationships: When Is It Ethically Acceptable to End Them?
Bioethics case study on doctor-patient relationships in VIDEO and PRINT. This case study in clinical ethics discusses when it is acceptable to end a doctor-patient relationship. Published by the Center for Practical Bioethics.
-
Case Study: Behavioral Issues Lead to Challenging Discharge
Bioethics case study on Mr. Ankeal with end-stage renal disease (ESRD) and multiple other chronic conditions, including chronic pain has been hospitalized. He has been moving between outpatient dialysis centers for several months due to repeated behavioral issues. The hospital care team has been unable to find an outpatient dialysis clinic willing to accept him due to his documented behavioral history. Published by the Center for Practical Bioethics.
-
Ethics Dispatch July 2025
The July Ethics Dispatch is on Why Rural Healthcare Fails Without Medicaid: An Ethical Analysis. With Medicaid cuts looming, we discuss the principles of bioethics to the cuts’ impact on rural healthcare. And we explore the philosophical concept of “ought implies can,” which holds that for someone to have a moral obligation, that person must have the ability to accomplish said obligation. Which begs the question: When do we have a moral obligation to provide Medicaid coverage?
.
-
Case Study – Distributive Justice: A Challenge for Clinical Ethics
Bioethics case study on distributive justice in VIDEO and PRINT. This case study in clinical ethics challenges several concepts within the idea of justice. Should this patient receive an equal share? Or receive according to his need? How do we ensure we treat this patient fairly?
-
Case Study: When is it ethical to override a patient’s medical wishes?
Bioethics case study on Mr. Schumann, who signed an advance directive seven years ago indicating that he would not want life-sustaining treatment if he were unconscious with no hope of recovery. The family acknowledges the directive but insists that, if he could speak today, he would want everything done – for their sake.
-
Case Study: Autonomy and Moral Distress Father Trent Chooses to Reject a Kidney
Bioethics case study on Fr. Trent’s request presenting a complex ethical dilemma involving organ allocation policy, personal autonomy, and the role of altruism in life-saving medical decisions.
-
Case Study – Immigrant Caregiver Mother Fears Visit to Hospital
Bioethics case study in which Eve’s mother, Gloria, is her primary caregiver and sole means of transportation to medical appointments. An immigrant from a foreign country, Gloria has been hesitant to accompany her daughter to the hospital. Fearing potential issues with the U.S. Immigration and Customs Enforcement (ICE), Gloria is afraid to visit the hospital, which in turn prevents her from driving Eve to her chemotherapy appointments.
-
Case Study – Should a Dying Patient Receive Pain Medications or Donate Organs?
Bioethics case study on a dying patient receiving pain medication OR donate organs in VIDEO and PRINT. Should we allow the patient to have a peaceful passing, but not allow them to donate organs which the patient had expressly stated they wanted to do?